

September 24, 2024
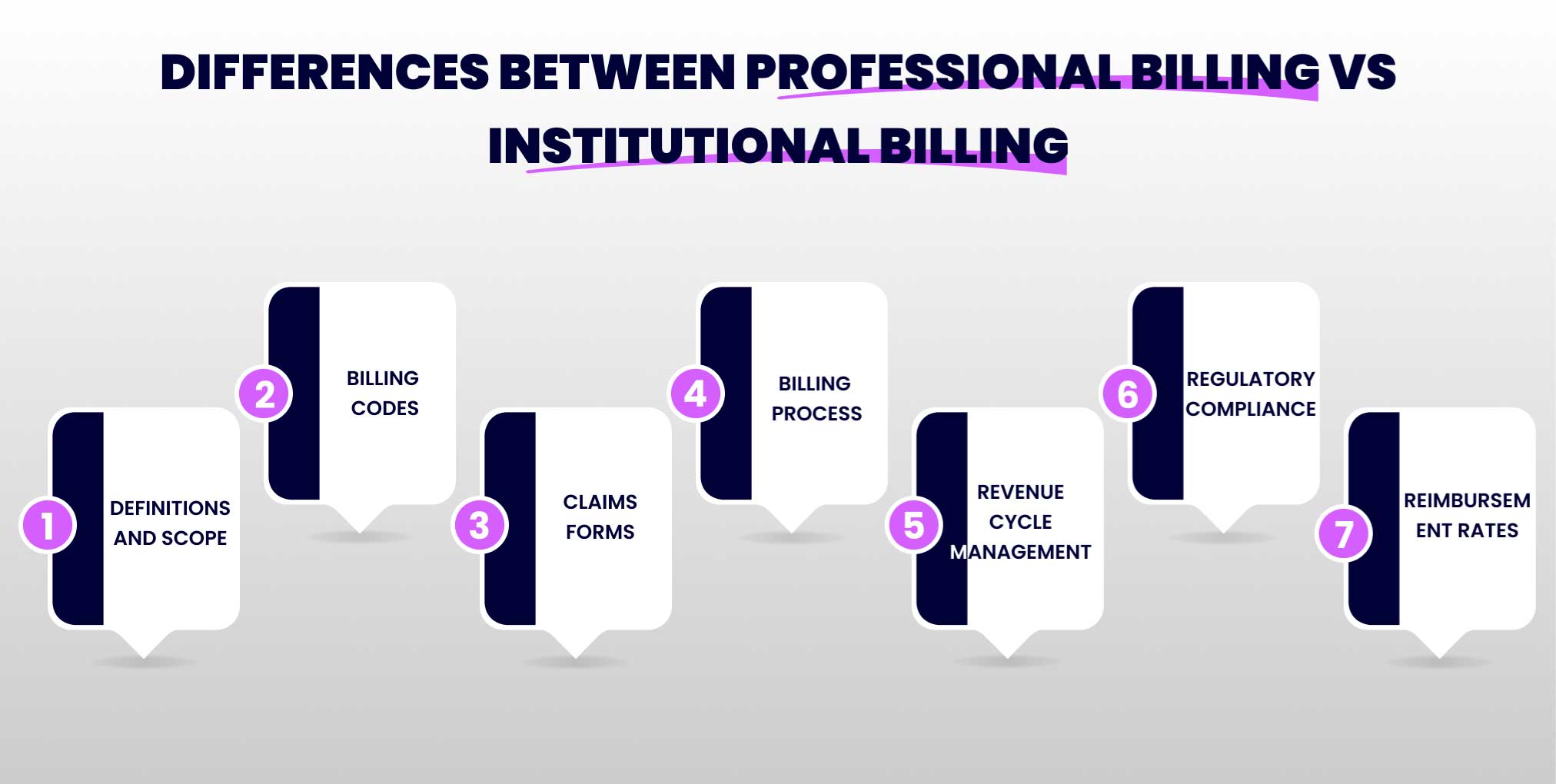
When it comes to the healthcare industry, many different terms and phrases can be confusing for those outside of the field. One common dilemma is understanding the difference between professional billing and institutional billing. While both types of billing are essential for ensuring proper payment in the healthcare system, they have distinct differences. In this blog, we will discuss professional billing vs institutional billing and provide a clear understanding of each.
If you want to work with a medical billing service, understanding the distinctions between institutional and professional billing is important. Without this understanding, you risk claim denials and potential revenue loss.
Professional billing is also known as physician or provider billing. It refers to the process of submitting claims for services provided by individual healthcare professionals such as doctors, nurses, therapists, etc. These services can include consultations, procedures, and any other medical services provided to patients. Professional billing is usually done by a third-party medical billing company or the in-house billing department of the healthcare provider.
Institutional billing is also known as facility or hospital billing. It involves submitting claims for services rendered in a healthcare facility, such as hospitals, nursing facilities, and outpatient clinics. These services can include inpatient and outpatient procedures, tests, medications, and other medical services provided to patients. Institutional billing is usually handled by the healthcare facility’s finance department or a third-party billing company.
Professional Billing
Professional billing is concerned with the claims process for individual healthcare providers. This includes services rendered by doctors, surgeons, anesthetists, and other healthcare professionals who provide direct patient care. These services are typically billed using the CMS-1500 form.
Institutional billing
Institutional billing covers the claims process for services provided by healthcare institutions. This includes hospitals, skilled nursing facilities, and other healthcare organizations. Institutional billing includes a wider range of services, such as inpatient care, outpatient services, diagnostic tests, and facility fees. The UB-04 (also known as CMS-1450) form is used for institutional billing.
Professional Billing
Institutional Billing
Professional Billing
Institutional Billing
Professional Billing Process
Institutional Billing Process
Professional Billing
Revenue cycle management (RCM) in professional billing involves an improved process to ensure that healthcare providers are reimbursed for the services offered. The focus is on efficient handling of outpatient services, timely submission of claims, and effective follow-up on denied or underpaid claims. The use of accurate CPT and HCPCS codes plays a critical role in reducing errors and ensuring quick reimbursement.
Institutional Billing
In institutional billing, RCM has a broader and more complex array of services. It includes managing inpatient and outpatient services, facility fees, and ancillary services. The emphasis is on capturing all charges accurately, ensuring compliance with coding standards, and managing high-volume claims. Effective RCM in institutional billing helps healthcare facilities maintain financial stability and support comprehensive patient care.
Professional Billing
Compliance in professional billing involves adhering to regulations set by entities like the Centers for Medicare & Medicaid Services (CMS) and private insurers. It includes accurate coding, maintaining patient confidentiality, and following proper claim submission protocols. Regular audits and training can help ensure compliance and reduce the risk of fraud and abuse.
Institutional Billing
Institutional billing compliance is more complex due to the extensive range of services billed. Institutions must adhere to federal, state, and payer-specific regulations. This includes compliance with HIPAA, the False Claims Act, and other regulatory requirements. Ensuring compliance in institutional billing helps avoid legal issues and ensures the proper handling of patient data and billing information.
Professional billing
Reimbursement rates are based on contracted fee schedules or negotiated rates between the provider and payer. Institutional billing: Reimbursement rates are predetermined by government agencies such as CMS, which can be subject to change.
Institutional billing
Reimbursement rates are predetermined by government agencies such as CMS, which can be subject to change.
Next time you encounter the terms Professional Billing vs Institutional Billing, remember their key features, differences, and importance in the healthcare industry. Professional and institutional billing are both important for the financial stability of healthcare providers. Understanding the two concepts can help you maximize your reimbursements and ensure efficient billing processes.
As the healthcare industry continues to evolve, it is essential to stay updated on any changes in regulations and guidelines for both types of billing. So, it is important to choose a reliable medical billing company to handle billing processes efficiently. By doing so, healthcare providers can focus on providing quality care to their patients without worrying about complex billing processes.